The journey to alcohol recovery can be successfully navigated through three main pathways, each offering unique opportunities for personal growth, fulfillment, and freedom from the burden of alcohol use disorder (AUD).
This compelling article explores a range of practical pathways to recovering from severe alcohol problems.
I’m thrilled to provide you with a Comprehensive and Impactful “Menu” of Categorized Resources for Alcohol:
- Safe and Comfortable Detoxification
- Withdrawal Symptoms Alleviation
- Craving Reduction
- Recovery and Healing
- Relapse Prevention
- Transcendence!
By meticulously categorizing and organizing these resources, I aim to simplify navigating the many options available.
It’s crucial to understand that there are dozens of specific pathways to recovery within these three main categories.
Let’s kick things off with a concise overview of alcohol use disorder and the most comprehensive definition of addiction, developed by addiction expert, speaker, and best-selling author Dr. Gabor Maté.
Following that, you will be guided through The 3 Pathways to Alcohol Recovery and offered expert advice on selecting the most suitable resources and pathways tailored to your unique needs and preferences.
What is Alcohol Use Disorder?
According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), “Alcohol use disorder (AUD) is a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences.”
“It encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, alcohol addiction, and the colloquial term, alcoholism.”
Throughout this piece, I will typically use the terms alcohol use disorder and AUD.
The Diagnostic Statistical Manual of Mental Disorders, 5th Edition (DSM-5) shows that to have a diagnosis of AUD, an individual needs to meet:
- Two criteria out of the list below for mild AUD
- 4-5 criteria for moderate AUD
- At least 6 of the criteria for severe AUD
DSM-5 Criteria for an Alcohol Use Disorder Diagnosis:
- Consumed more alcohol or spent more time drinking than intended.
- Want to limit or halt alcohol use, but haven’t succeeded.
- Spends an inordinate duration drinking, being ill and undergoing the aftereffects of alcohol use.
- Consuming alcohol or becoming ill because of it has kept the person from properly attending to household duties and children, or resulted in difficulties performing on the job or at school.
- Continued drinking in spite of it causing problems with family and loved ones.
- Discontinue or are only sporadically involved with things that were once enjoyable or important to be able to drink.
- Have repeatedly been in situations during the consumption of alcohol that have increased the chance of being injured (using machinery, driving).
- Even though a person feels sad or distressed, or it affects an already existing health problem, the person continues to drink. Or after episodes of forgetting or going blank about the events during drinking, the individual continues to use alcohol.
- Have to increase drinking to get the results he wants. (The usual amount of alcohol provides little results).
- When alcohol wears off, causing symptoms like such as insomnia, difficulty staying asleep, aggravation, nervousness, sadness, stomach upset and nausea and/or perspiring.

A New Working Definition of Addiction
Dr. Gabor Maté has introduced a compelling new definition of addiction, which he asserts is more precise and influential than previous definitions.
I fully support his perspective and am enthusiastic about sharing it with you for your thoughtful consideration.
Here is what Dr. Maté’s new working definition of addiction says:
“Addiction is a complex psychological, emotional, physiological, neurobiological, social, and spiritual process. It manifests through any behavior in which a person finds temporary relief or pleasure (and therefore craves) but that, in the long term, causes them or other negative consequences, and yet the person refuses or is unable to give it up.“
— The Myth of Normal: Trauma, Illness & Healing in a Toxic Culture
Accordingly, Dr. Maté’s definition includes three main hallmarks of addiction:
- Short-term relief and pleasure (and therefore craving)
- Long-term suffering for oneself or others
- And an inability to stop
You might have noticed that Dr. Maté’s definition omits “disease,” but that does not mean it must exclude it.
He says that “most illnesses are best understood as complex processes manifesting a person’s entire life rather than discrete things and that in the end, as with many conditions, calling addiction a disease may capture relevant aspects of it without coming close to explaining the phenomenon, let alone granting us a workable pathway to healing it as its source.”
Now that you have a little background on AUD and a more expanded view of addiction as a whole, let’s move on to pathways to recovery, starting with what is referred to as the Clinical Pathways to Recovery.
1. Clinical Pathways to Alcohol Recovery
Clinical Pathways to Recovery involves professional intervention from a healthcare provider, clinician, or other credentialed professional.
Here are some compelling examples of Clinical Pathways to Alcohol Recovery…
Clinical Treatment
In medically monitored inpatient detoxification and clinically managed residential services, you are supported by a team of dedicated physicians, counselors, therapists, and other professionals as you spend each day and night in treatment, typically lasting 3-90 days.
Moreover, intensive outpatient and partial hospitalization programs, as well as outpatient services, are available, allowing individuals to receive treatment for AUD while remaining at home.
This lower level of care (LOC) is ideal for individuals who do not need the higher level of care provided by inpatient detoxification and rehabilitation, which offers 24/7 care.
Pharmacotherapy and Medication-Assisted Treatment
Having personally experienced the challenges of alcohol withdrawal symptoms, cravings, and insomnia, I understand the immense difficulty it presents.
I have faced severe alcohol withdrawal on numerous occasions, and without the aid of withdrawal medications, the outcome could have been fatal. It’s crucial to recognize that while prescription drugs can be beneficial, some can also be habit-forming or addictive, and all medications come with potential side effects.
A diligent pros/cons and risk/reward analysis can help you discern whether this pathway is viable.
Medications that hold FDA approval for the treatment of AUD include:
- Naltrexone (oral and injectable)
- Acamprosate
- Antabuse
There are also off-label options such as:
- The Sinclair Method (TSM)
- Librium
- Trazodone
- Gabapentin
- Topamax
Many other off-label uses of medications can often help ease the difficulties of quitting alcohol. Remember, you’re not alone in this; options are available to support you.

Behavioral Therapy
Many people seek help for alcohol use disorder from a reputable therapist who specializes in working with this condition.
Working with a therapist can provide valuable support and guidance on your journey toward recovery, especially one who practices:
- Acceptance and Commitment Therapy (ACT) — Teaches individuals to accept challenging situations rather than avoiding them. It has been successful in reducing various mental and substance use disorders.
- Cognitive Behavioral Therapy (CBT) — Has among the highest levels of empirical support for the treatment of drug and alcohol use disorders.
- Motivational Interviewing (MI) — Focuses primarily on increasing motivation and also has among the best validated and most widely disseminated of all psychosocial interventions for alcohol use disorders.
- Family Therapy — Involving family members in therapy increases the individual’s likelihood of staying in treatment. Family members can be a positive force while supporting their loved one’s recovery.
Moreover, I recently read a book about a cutting-edge type of psychotherapy for AUD called Internal Family Systems (IFS), which helps people understand and heal their mental system’s different parts or sub-personalities.
IFS therapy is an evidence-based practice that can help people with alcohol use disorder and other substance use disorders.
IFS therapy can help people recover from alcohol use disorder by:
- Building relationships: Helping people build relationships with their core Self and different parts of themselves
- Understanding parts: Helping people understand the origins and function of these parts
- Integrating and healing: Guiding people towards integrating and healing these parts
- Increasing self-awareness: Helping people increase their self-awareness and emotional regulation
- Improving overall wellbeing: Helping people improve their overall wellbeing

Holistic Therapies
Another term for this is ‘Integrative Health,’ which involves integrative and complementary healing modalities to integrate or assimilate the whole person (mind, body, and spirit) to promote and facilitate overall wellness and harmony.
Some of the most commonly used holistic therapies include:
- Mindfulness
- Meditation
- Massage Therapy
- Acupuncture
- Yoga
- Reiki
- Music and Art Therapies
- Aromatherapy
- Animal-Assisted Therapies
- Hypnosis

Now that we’ve covered the Clinical Pathways to Recovery, it’s time to discuss the most popular recovery pathway…
2. Non-Clinical Pathways to Alcohol Recovery
The second category of Pathways is Non-Clinical. Non-Clinical Pathways to Recovery are the most utilized, accounting for slightly more than 50% of preferred Pathways.
Non-clinical pathways represent recovery processes that:
- Do not involve a Clinician
- Utilize no formal services
- Nearly always involve Community-Based and Peer Support-Based Pathways.
Some popular Non-Clinical Pathways to Recovery are…
Recovery Residencies
Recovery Residences, also known as ‘Sober Homes,’ ‘Sober Living Homes,’ or ‘Halfway Houses,’ are non-medical settings designed to support recovery in a substance-free environment.
They are commonly used as a transitional bridge from:
- Residential treatment-to-employment
- Obtaining more permanent residence
Recovery Community Centers
Recovery Community Centers (RCCs), also known as ‘Recovery Cafes’ or ‘Recovery Support Centers,’ are Peer-Operated Centers that support building Recovery Capital.
Recovery Capital is defined as “The breadth and depth of internal and external resources that can be used to initiate and sustain recovery or wellness from severe alcohol or other substance use disorders.”
Education-Based Recovery Services
Education-Based Recovery Support Services are tailored to help individuals achieve their educational goals while simultaneously addressing their social, emotional, spiritual, and physical well-being to sustain recovery.
Examples of these services include:
- Recovery High Schools—Provide a supportive environment for students in recovery.
- Collegiate Recovery Programs—Offer peer support and guidance to help students manage their recovery while pursuing their education.
The main goal of Education-Based Recovery Services is to help students maintain positive behavior change and sustain their recovery.
Employment-Based Recovery Services
These are programs set up by employers to facilitate employment and workforce training for individuals in recovery from substance use disorder.
They help current employees access resources and treatment for substance use disorder.
According to a study, people who find jobs while in recovery have lower relapse rates.
People in recovery also often give back to their communities at a rate about double the general population.
Self-Help Groups
Last but not least, we now cover the popular Peer-Based Recovery Support, also known as Self-Help Groups or Mutual Aid Organizations.
There are also three categories of Self-Help Groups:
- Twelve-Step Groups — Alcoholics Anonymous, Narcotics Anonymous, etc (spiritual program or ‘fellowship’).
- Secular Groups (Non-Twelve-Step) — These are much less utilized than Twelve-Step, but they’re growing fast, especially SMART Recovery, Life Ring, and Women for Sobriety.
- Faith-Based (or Faith—and Culture-Based Recovery Support) Organizations — These are much less utilized than Twelve-Step groups, but they’re also growing fast. Celebrate Recovery is a famous example.

Finally, we come to the third and final category of alcohol recovery pathways, which is known as Self-Management Pathways.
3. Self-Management Pathways to Alcohol Recovery
The Self-Management Pathway category is also known as ‘Self-Directed’ or ‘Self-Managed’ and is less commonly called ‘Natural Recovery.’
This category encompasses recovery processes that:
- Do not involve formal recovery programs
- Do not engage with professional services
- Do create their own path
In self-directed or natural recovery, individuals have the freedom to chart their own course on the path to alcohol recovery.
My Self-Managed Alcohol and Other Drug Recovery Journey
After failing at addiction recovery for ages when trying Clinical, Non-Clinical, and Self-Management Pathways, I finally found a path forward that worked great for me.
After doing a medication-assisted detox from home using physician-prescribed pharmacotherapy (Clinical Pathways) and then only 30 days of AA meetings (Non-Clinical Pathways), I began my Self-Directed Pathway to Recovery.
I found immense success forging this path using Natural Recovery when I attempted it at age 32.
It worked well for me because I’ve been addiction-free for over 12 years. Here are some real-life examples of natural recovery or self-management pathways to recovery.
On my 31st day of recovery, I confidently initiated a journey that included the following habits:
- Brain and Body — Health and Wellness, Nutrition, Supplementation, Physical Fitness, Surfing, Hiking, and more.
- Mind and Emotions — Personal Development, Journaling, Reading 1-2 Non-Fiction Books a Week, Mindset Training, Resilience Training, and more.
- Spirit and Fulfillment — Growth and Contribution, Service to Others, Prayer, Meditation, Mindfulness, Qigong, Yoga, Camping in Nature, and more.
- Relationships and Home — Family Support, Sober Friends, Disassociated from Drinking/Drugging Friends, Home Conducive to Recovery (Alcohol and Drug-Free Parent’s Home), and more.

Chris Scott’s Self-Managed Alcohol Recovery Journey
Chris Scott, the founder of Fit Recovery and co-creator of the Fit Recovery 2.0 Membership Program, used Clinical Pathways of Recovery when he went through a medical alcohol detox followed by a 30-day residential inpatient treatment that focused on Twelve-Step recovery (Non-Clinical Pathways).
After Chris graduated from treatment, he also forged a Self-Directed Path to Alcohol Recovery that closely mirrored my Natural Recovery process.
Chris also diligently cultivated the following new habits for alcohol recovery:
- Devoting time to health and wellness, fitness, and supplementation
- Reading 1-2 non-fiction books weekly
- Working on self-development
- Focusing on optimizing mental and emotional well-being
- Maintaining a healthy family and friend support system
- Prioritizing long-range goals versus instant gratification
- Being highly proactive
- and more!
While my focus was primarily on engaging in surfing for fitness, Chris directed his efforts toward performing heavy deadlifts at the gym. Regular, vigorous exercise helped us both feel and look our best, making it easier to avoid alcohol.

Which Pathway to AUD Recovery Should I Choose?
So, what is the best path to recovery? Well, despite what a small percentage of AA members say, there is no best path to recovery, and there is undoubtedly no one path only to recovery.
The fact is…
The concept of “recovery” encompasses a wide range of paths and ideas, all of which can vary significantly depending on the individual.
Each person is highly unique, and thus, different pathways of recovering will resonate with different people depending upon their:
- Severity of alcohol use disorder
- Length of AUD
- Age
- Physical health and vitality
- Mental health
- Personality
- Demographics
- Psychographics
- Culture
- Gender
- Race
- Values
- Belief in religion, spirituality, or none
- Co-occurring or ‘concomitant’ disorders or none
- Resources
- Finances
- Insurance
- Recovery Capital
- Amount of stress
- Lifestyle
- Location
- Relationships and social dynamics
- Family dynamics
- Work dynamics
Along with this list, numerous other variables contribute significantly to each individual’s unique situation.

Completing an online Recovery capital assessment is one of the most strategic first steps in determining which pathways to consider.
The Recovery Capital Scale
Recovery Capital (RC) is the breadth and depth of internal and external resources that can be drawn upon to initiate and sustain recovery from severe AOD problems (Granfield & Cloud, 1999; Cloud & Granfield, 1 Page 2, 2004).
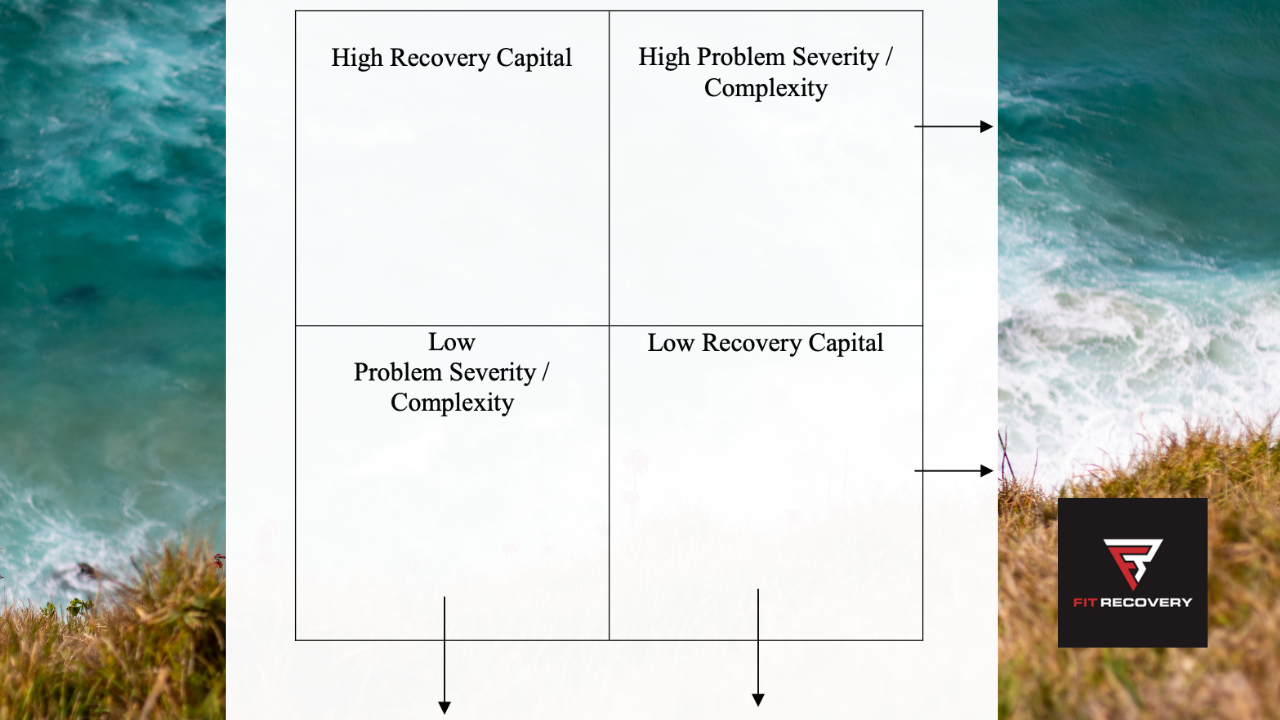
An individual with a low-severity alcohol use disorder can typically recover with low recovery capital. In contrast, a person with a severe alcohol use disorder usually requires high amounts of recovery capital to heal.
The Recovery Capital Scale is a free online assessment that can help you gauge your progress and show your strengths, improvement areas, and total recovery capital score. The more recovery capital you have, the easier and smoother it will be to overcome alcohol use disorder and recover in body, mind, spirit, relationships, finances, etc.
Robert Granfield and William Cloud introduced and explained the concept of “recovery capital” in their 1999 book, Coming Clean: Overcoming Addiction without Treatment.
They define recovery capital as:
“The internal and external assets that can help initiate and maintain recovery from alcohol and other drug problems.”

Recovery capital varies from person to person and can change within the same person over time. It also interacts with the severity of the problem to determine the level of support needed for recovery.
This interaction influences the intensity of professional treatment and the duration of post-treatment recovery support services required for each individual.
Clients with more severe problems but substantial recovery resources may need less help to start and continue their recovery than those with fewer problems and few recovery resources.
The first group may benefit from the following:
- Outpatient Counseling
- Recovery Coaching
- Connecting with Recovery Support Groups
- Some ongoing supervision and accountability
The second group may need:
- More intense treatment
- More involvement in a recovery-focused community, such as:
- Living in a recovery home
- Participating in support groups
- Joining recovery-oriented social activities
- More careful ongoing monitoring and supervision
The figure below (from the Recovery Capital Scale assessment) shows how problem severity and recovery capital combinations could vary.
Check out the Multidimensional Inventory of Recovery Capital (MIRC) to learn more and utilize a second resource.
It was created by a multidisciplinary team of researchers—led by Elizabeth Bowen, PhD, an associate professor in the University at Buffalo School of Social Work—with funding from the U.S. National Institute on Alcohol Abuse and Alcoholism (NIAAA).
10 Key Concepts of Pathways to Alcohol Recovery
Now that you’ve discovered the three categories of pathways and many of the specific roads to recovery within the categories, it’s time to review the key concepts.
Therefore, you will absorb the crucial aspects of this training on how to overcome alcohol use disorder.
Here are the fundamentals for you to meditate on:
- Alcohol use disorder (AUD) is a complex psychological, emotional, physiological, neurobiological, social, and spiritual process characterized by an impaired ability to stop or control alcohol use despite adverse consequences.
- Recovering from AUD can be done through three main pathways.
- Clinical pathways to recovery involve professional intervention from a healthcare provider, clinician, or other credentialed professional.
- Non-clinical pathways are recovery processes that do not involve a clinician. They typically involve community-based and peer support-based pathways without formal services.
- Self-management pathways do not involve formal recovery processes or engagement in professional services (“choose your own path” recovery).
- Despite what a small percentage of AA members say, there are many paths, roads, and ideas about recovery.
- Every individual is unique, and as such, the journey to alcohol recovery must be tailored to resonate with each person’s specific circumstances and needs.
- The level of care (LOC) is based on individual needs and can range from early intervention to intensive inpatient care. The American Society of Addiction Medicine (ASAM) Criteria guide the determination of the necessary level of care.
- Recovery capital (RC) is the breadth and depth of internal and external resources that can be drawn upon to initiate and sustain recovery from severe AOD problems.
- You can use the Recovery Capital Scale to gauge your current recovery capital and identify areas for improvement.
If you have any comments or questions, please post them in the comment box below. Take good care of yourself, and make sure to check out our new article on how Accountability de-activates alcohol addiction.
You’re going to be really happy that you took action!
“Accountability multiplied by Recovery Capital = AUD Recoverability Potential.” — Matt Finch
Author
-
Matt Finch, the Fit Recovery Head Coach, embodies the power of transformation. With over 13 years of freedom from both alcohol and opioids, he has turned his personal journey into a beacon of hope for others. Previously a Certified Substance Abuse Counselor at an outpatient treatment center, he has dedicated his life to empowering individuals to break free from the chains of addiction. Through his innovative recovery coaching programs, he has joined forces with Chris Scott and Fit Recovery, inspiring thousands to overcome their struggles. By offering one-on-one recovery coaching, engaging group sessions, and dynamic online courses, along with his uplifting podcast, "The Matt Finch Show: Fit Recovery 2.0 Members-Only Alcohol-Free Lifestyle Podcast," he illuminates a path to a healthier, addiction-free lifestyle.
View all posts Fit Recovery Head Coach