The purpose of this article is to shed light on the relationship between naltrexone and alcohol, including the concept of pharmacological extinction.

Overview
Naltrexone hydrochloride is a medication that has been approved to treat opioid addiction for decades, and addiction since 1994. This is the generic name for this drug, and brands include an oral pill called Revia and a long-acting shot called Vivitrol.
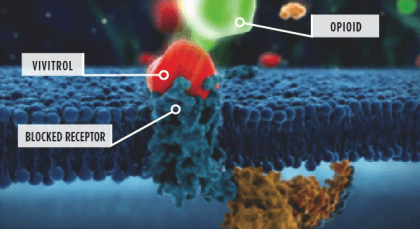
It is an opioid antagonist, meaning that it plugs the same brain receptors as opiates and endorphins (the brain’s natural pleasure chemicals). Instead of producing pleasurable effects, it sits in the receptor site and simply blocks pleasure chemicals from entering.
Specifically, this medication plugs the mu-opioid beta-receptor. You can see how this works in the picture below, which portrays the action of the Vivitrol shot.
When alcohol is consumed, the brain releases endorphins, which are endogenous opioids that are also released in response to exercise, food, sex, and other pleasurable activities.
It prevents drinkers from feeling pleasure when they drink. When the oral pill version is consumed, it must be taken before every drinking session to be effective.
This medication was approved for addiction in 1994 after studies demonstrated that it reduced the amount of drinking and the severity of relapses.
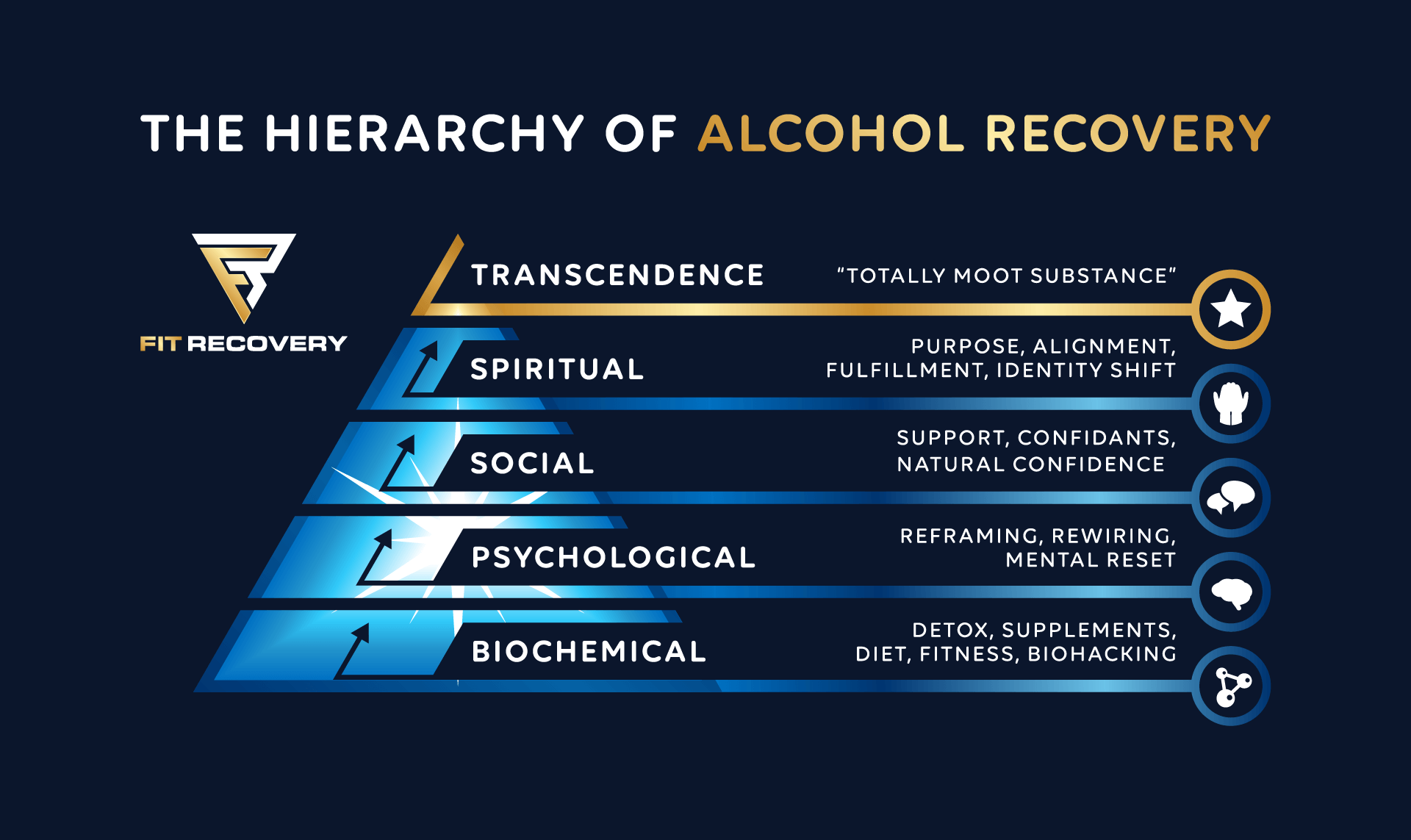
Importantly, taken alone with abstinence shows only a small reduction in relapse rates. The mechanism through which it works requires naltrexone and alcohol to both be present, over the course of repeated episodes of drinking. This process is called pharmacological extinction.
Pharmacological Extinction
In other articles, we’ve partially explained addiction as an attempt to maintain comfortable levels of GABA, which is the brain’s primary calming neurotransmitter.
Yet as any heavy drinker knows, the calming effect of liquor is only half of the equation. The other half is the profound sense of pleasure, euphoria, and reward that our brains come to associate with drinking.

For people who are actively addicted, nothing releases endorphins as intensely as large quantities of alcohol.
In the past few decades, scientists have concluded that alcohol’s effects are mediated at least partly through the brain’s internal opioid system. This system is closely connected to the dopamine system, which is responsible for learning, motivation, and sense of reward.
From an evolutionary perspective, this makes sense: We need to remember things in our environment that give us pleasure so that we can instinctually seek them out in the future. For people with addiction, the brain’s attempts to automate goal-seeking ends up threatening survival itself.
The progression of drinking can therefore be seen as a learned behavior even though the drinker has no conscious control over it. This kind of subconscious learning is reinforced by a chain reaction of neurotransmitters beginning with endorphins, which eventually causes the brain to release dopamine at the very idea of drinking. For an addict in withdrawal, a single thought can easily begin the process of getting ready to go obtain alcohol from a store or a bar.
Pharmacological extinction is the gradual reversal of drinking as a learned behavior. It is made possible by the repeated presence of both, allowing the drinker to stop feeling pleasure and euphoria from the act of drinking. Over time, the drinker’s internal opiate system and dopamine system rewire so that the thought of alcohol produces a state of indifference rather than craving.
In a sense, pharmacological extinction is the addict equivalent of training Pavlov’s dogs to associate the bell with no food at all (i.e., no salivation or cravings).
Pharmacological extinction requires that both are taken together for as long as the person decides to drink. In other words, for people who use this medication for addiction, it should be taken before each drinking session for the rest of their lives.
If they simply stop taking it and continue to drink, endorphins will be released that could rekindle their addiction all over again.
Research Studies

Over the past few decades, a lot of research has been done. The use of naltrexone for alcohol disorders is well-established in the scientific literature:
- In a 6 month double-blind, placebo-controlled study with 118 alcoholics, naltrexone was associated with significantly fewer heavy drinking days than the placebo (source)
- A 1997 study found that when this medication was combined with therapy, only 35% relapsed, compared to the treatment industry standard of up to 90% relapse (source)
- Out of 14 clinical trials conducted through 2001, only two failed to demonstrate the efficacy of naltrexone for alcohol disorders (source)
- A 2014 meta-analysis found it effective at reducing heavy drinking and extinguishing cravings (source)
- People with a particular variant of a gene (A118G Asn40Asp, or asparagine-to-aspartate amino acid substitution at position 40) for the mu opioid receptor obtain a greater high from drinking and more dopamine response. A study conducted on alcoholics with this genotype found more success using naltrexone for addiction (in the form of reduced return to heavy drinking) than with other genotypes. (source)
The last study points to a recurring theme on this site: Due to biochemical individuality, some treatment methods work better for some people than for others.
How To Use

The following information may be useful if you are considering:
- This is a generic drug, and the two main brand names are Revia and Depade.
- Revia comes in bottles of 30 or 100 tablets, 50 mg each, while Depade comes in bottles of 30 or 100, either 25, 50, or 100 mg each.
- Typical dosage is 25-50 mg per day, either once per day, in split doses, or just prior to drinking.
- For long-term users, the drug only needs to be taken prior to drinking.
- It has a low incidence of adverse effects that force people to stop using the drug; however, side effects can occur.
- Only take it under the supervision of a doctor.
Note: In severe cases, as defined by high consumption and drinking, detoxification with medications may be necessary before introducing this medication for addiction and attempting to achieve pharmacological extinction. Usually, 3-7 days of abstinence are recommended before treatment. (source)
Before taking it, make sure to review the following:
Alternative Treatment Methods
Not everyone can obtain a prescription. Fortunately, more doctors are becoming aware of this relationship.
While a unique form of harm reduction, there are alternatives – including drugs that have been shown to be effective in controlling cravings when administered for long periods of time.
Baclofen
Baclofen is a prescription drug that is structurally similar to GABA. Baclofen can be used to manage withdrawal symptoms, and it has also been used long-term by a growing number of people to achieve a state of indifference toward alcohol.
To learn more, check out on the interesting baclofen alcohol relationship.
Gabapentin
Gabapentin is similar to baclofen in that it helps the brain produce more GABA. It is increasingly popular for withdrawal and sometimes combined with baclofen for long-term extinguishing of cravings.
You can read more about gabapentin in this article on this treatment method.
Conclusion
Naltrexone for addiction is a little-known but highly effective treatment that our medical establishment has all but hidden from patients. While not everyone responds well, greater awareness of this relationship can improve recovery odds for many people.
There is no one-size-fits-all approach to detox and recovery. Most people who quit drinking are not enlightened about other pharmacological options, nutrient repair, the hypoglycemic trap that so many people fall into, or holistic strategies for improving quality of life.
Check Fit Recovery’s list of supplements that work best for supporting the brain-body system through recovery.
If you have any questions, please leave them in the comment box below.
___________________________________
Dr. Ken Starr is board-certified in both Addiction Medicine and Emergency Medicine, and diplomate of the American Board of Addiction Medicine. In addition to his work as the Addiction Medicine Director for Fit Recovery, he operates Ken Starr MD Wellness Group in Arroyo Grande, CA. His clinic offers advanced drug and alcohol detox methods, long-term recovery facilitation, and IV nutritional programs including NAD+ therapy.
Author
-
Dr. Ken Starr is board certified in both Addiction Medicine and Emergency Medicine, and diplomate of the American Board of Addiction Medicine. In addition to his work as the Addiction Medicine Director for Fit Recovery, he operates Ken Starr MD Wellness Group in Arroyo Grande, CA. His clinic offers advanced drug and alcohol detox methods, long term recovery facilitation, and IV nutritional programs including NAD+ therapy.
View all posts






[…] Prescription-only drugs that have been FDA-approved for alcohol-use disorder (AUD) include naltrexone, acamprosate, and […]
Incredible article!!!
Thanks Chelssa!
I live in Nashville Tn and can not find anybody to help me with the Sinclair solution. I even email a rehab in Knoxville that says they use the Sinclair method and they never got back to me.
Hi Sondra, the C Three Foundation provides a resource for finding doctors familiar with Sinclair: http://www.cthreefoundation.org/find-a-physician.html#.VnnX686SOuU