This article will provide an overview of antidepressants and alcohol, exploring their effects and interactions. Many of our recovery coaching clients have been prescribed these medications, which they have been taking for years or even decades.

It’s alarming that the very real interactions between antidepressants and alcohol are not discussed more often. In our heavy drinking culture, many people drink frequently to “take the edge off” of life.
For the 1 in 6 Americans who take psychiatric medications, and who may also be slightly more predisposed to addiction due to mood disorders, heavy drinking can be a dangerous lifestyle choice.
Regardless of whether you take these, you don’t need liquor to enjoy life. Moreover, many people are able to become happy and thrive after quitting drinking without depending on prescription drugs.
We will now proceed to overview the effects on the brain. We also will cover some common questions about the effects of combining these drugs, the use of these medications after quitting, and some alternatives that can be used to enhance your sense of life and address long-term deficiencies in neurotransmitters, nutrients, and hormones.
Overview
Overview Of Alcohol
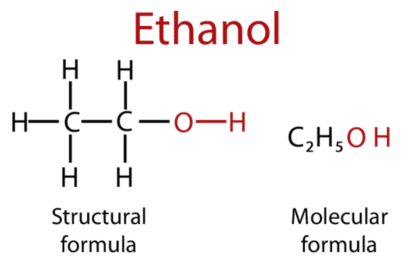
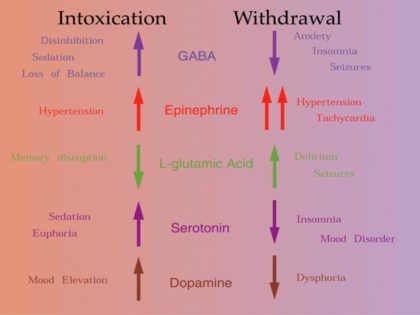
Alcohol is a central nervous system depressant that is very similar in structure to GABA, which is the brain’s primary calming neurotransmitter. It also activates the brain’s mu and kappa opioid receptors. (source) In turn, alcohol releases dopamine and raises levels of serotonin. Its effects on the brain are far-reaching and complex.
The most common side effects include:
- Relaxation
- Euphoria
- Disorientation
- Sedation
- Hangovers
- Dependence
How Alcohol Affects Serotonin
Alcohol causes an artificial spike in serotonin levels, which crash during withdrawal. As we will see, this is significant because many of these medications work by amplifying the effects of serotonin.
Because of biochemical individuality, different people respond to this substance in different ways. For people who become addicted, the effects of prolonged drinking can become very severe:
- High blood pressure
- Pancreas inflammation
- Liver cirrhosis
- Brain damage
- Damaged immune system
- Increased stroke risk
- Increased cancer risk
The liver breaks down alcohol into water, acetic acid, and acetaldehyde. This last compound is a poison that is responsible for hangovers and free radical damage to bodily cells, increasing inflammation and the risk of cancer.
Its addictive potential seems to strongly correlate with individual biochemical makeup, which is determined by genes – and which are, in turn, activated by environmental factors such as lifestyle. About 88,000 Americans die each year of alcohol-related causes. (source)
Overview of Antidepressants
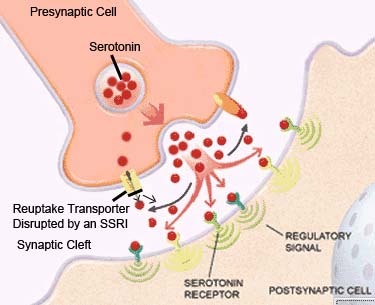
The most common form is selective serotonin reuptake inhibitors, often called SSRIs. Serotonin is a chemical and neurotransmitter that regulates mood, social behavior, digestion, and sleep.
In some cases, depression is caused by an insufficient supply of serotonin. SSRIs keep serotonin concentrated between the synapses instead of being taken back up into neurons. Serotonin and other neurotransmitters exert most of their effects – such as relaxation – between synapses, which are gaps between neurons.
The most common ones that fall into the SSRI category include:
- Prozac (fluoxetine)
- Zoloft (sertraline)
- Celexa (citalopram)
Others are serotonin and norepinephrine reuptake inhibitors, also called SNRIs. These drugs work on receptors for both serotonin and norepinephrine, which is another neurotransmitter whose deficiency can lead to depression. The most common brands that fall under this category are:
- Effexor (venlafaxine)
- Cymbalta (duloxetine)
When SSRIs or SNRIs do not work, tricyclic antidepressants (also called TCAs) are often prescribed. Scientists have not yet discovered the mechanism by which TCAs treat depression.
Side Effects

These medications can potentially have some pronounced side effects, including:
- Nausea
- Weight gain
- Loss of libido
- Fatigue
- Drowsiness
- Impaired vision
- Dry mouth
- Constipation
Most are known to cause dependence when used for extended periods of time. If these drugs are stopped abruptly, psychosis and suicidal ideation can result. The use of these has increased in recent years, with 13% of Americans taking some form of antidepressant. (source)
What Happens If You Mix?

SSRIs like Prozac and Zoloft (fluoxetine and sertraline) can cause tiredness, interfering with coordinated movement and alertness. Combining these types of medications with drinking can lead to extreme drowsiness and sedation.
More severe interactions include:
- Dizziness
- Drowsiness
- Fatigue
- Weakness
- Suicidal thoughts
Because Prozac and Zoloft are long-term drugs, interactions with alcohol can occur even if you don’t drink at the same time that you take the drug. It is recommended that people avoid drinking when taking Prozac.
Prozac may cause a slight reduction in the desire to drink, but this drug is not effective on its own for treating dependence.
SNRIs like Venlafaxine and duloxetine (Effexor and Cymbalta) react similarly when mixed with drinks. Alcohol and antidepressants in the SNRI category can interact in unpleasant ways, resulting in:
- Suicidal ideation
- Depression
- Anxiety
Scientists do not yet fully understand how tricyclic antidepressants interact with booze. Therefore, care should be taken when drinking while taking these drugs.
Can You Die From Mixing?
We have a silent epidemic of people who take antidepressants and also drink heavily. Due to the interactions listed above, this combination is potentially dangerous for mental health. Death from acute interactions is possible, but more commonly results from the consequences of increased drowsiness or psychological deterioration.
Combining these medications with drinks can indirectly lead to death through impaired vehicle operation, suicidal attempts, and other accidents. It’s also possible to overdose on SSRIs or Monoamine Oxidase Inhibitors (MAOIs) alone, resulting in high blood pressure or stroke. This risk is increased when drinking.
How Much Alcohol Can You Drink While On Antidepressants?

Many doctors believe it’s safe to drink lightly (1-2 drinks) while on these medications. Still, the aforementioned risks of combining these medications with alcohol should be kept in mind. Heavy drinking should be avoided, especially if you have risk factors for developing an addictions.
Heavy drinking leads to nutrient and neurotransmitter deficiencies, including serotonin and dopamine, which are targeted by many of these medications. They concentrate levels of neurotransmitters between the brain’s synapses, rather than restoring natural supply. Therefore, heavy drinking over time can increase the likelihood that an antidepressant stops working, with potentially dangerous or lethal outcomes.
Because many are metabolized by the liver, which also processes alcohol, combining them and drinking can lead to increased stress on the liver.
Do Antidepressants Increase Alcohol Tolerance?
They do not increase the tolerance for alcohol. Because these drugs can increase drowsiness when combined with liquor, it is advisable to drink less or not at all while taking them.
Because it is a depressant, it can negate the effects of antidepressants in some people. The negative effects of intoxication, including impairment of cognition and fine motor skills, can also become more pronounced in people who take these medications. Therefore they can decrease tolerance for some people, without directly influencing how much they decide to drink.
It’s worth noting that these medications have not been shown to help people with addiction stay abstinent. Prescription-only drugs that have been FDA-approved for alcohol-use disorder (AUD) include naltrexone, acamprosate, and disulfiram.
If you take an antidepressant, it’s a bad idea to skip your medication dose to drink. Stopping abruptly can result in adverse psychological reactions.
Supplements To Avoid While On Antidepressants
Due to possible interactions, people who take these should always consult their doctor before taking supplements.
Of particular concern are interactions between SSRIs, which artificially concentrate a person’s existing supply of serotonin between their synapses, and amino acids like L-tryptophan and 5HTP that are natural precursors for serotonin.
In rare but documented cases, combining SSRIs with L-Tryptophan or 5HTP can cause serotonin syndrome, which can be potentially fatal.
With that said, clinicians have successfully weaned people off of them with the help of these amino acids. This should always be performed under the guidance of a doctor.
As a rule of thumb, SSRIs should not be combined with the following supplements:
- L-Tryptophan
- 5HTP
- SAMe
- Garcinia Cambogia
For people who take SSRIs, care should also be taken with dosages of B-vitamins, Vitamin E, and Vitamin K. These basic nutrients are involved in regulating mood and the absorption of tricyclic medications.
If you are uncertain as to whether your antidepressant will interact with a given supplement, consult your doctor. If you do not have access to a doctor, you can also Google “[antidepressant name] and [supplement name]” and refer to trusted sources such as WebMD.
Use of Antidepressants For Alcohol Dependence

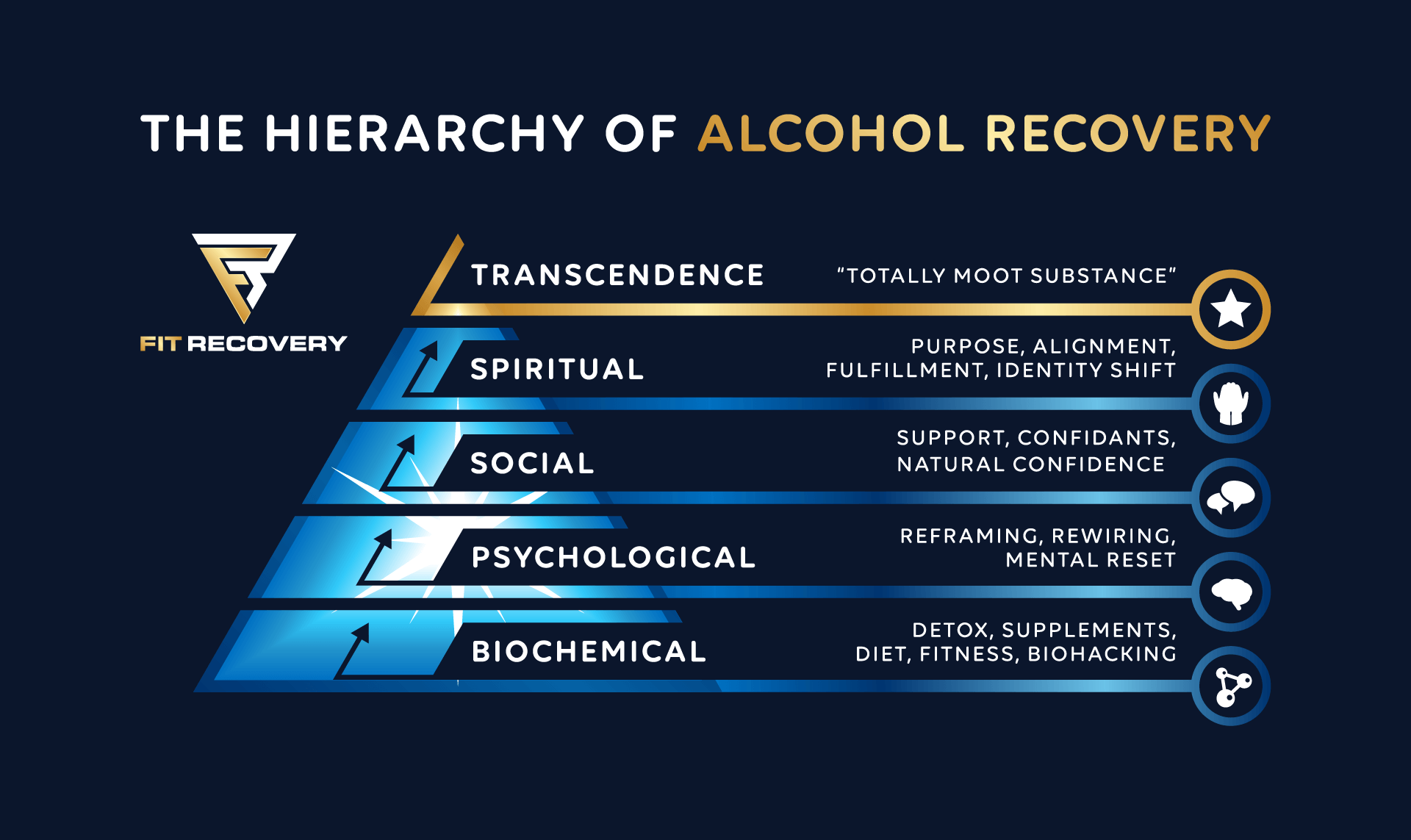
These medications are not effective in preventing relapse into addiction. This is likely because drinking affects a much wider range of neurotransmitter systems than serotonin or norepinephrine.
However, some people do report that they help them to minimize the depression that often accompanies post-acute withdrawal syndrome. Others use natural methods such as serotonin-boosting supplements 5HTP and L-Tryptophan, which do not need to be continued forever.
Some people benefit from taking long-term. However, up to 30% of people on these medications either do not respond to these drugs or find that they cause more harm than good. (source)
It’s not uncommon for people on these to experience complacency at inappropriate times or a reduced zest for life. Dig deep enough, and you’ll inevitably come across stories of people who felt nothing at funerals for family members – or who felt nothing but “flat” during moments that should have been the happiest in their lives.
Other people experience an initial benefit that wanes with time, leaving them dependent on prescription drugs that keep them at baseline without enhancing their lives.
Many people who have struggled with depression for their whole lives are beginning to find that exercise, diet changes, and natural supplementation work to alleviate the chronic deficiencies in neurotransmitters that cause depression.
Alternatives
Studies have shown that exercise can reduce depression as effectively, and doctors have even begun prescribing exercise to depressed patients. As it turns out, exercise helps the brain rewire itself away from alcohol addiction.
Natural supplements, such as L-Tryptophan and 5HTP mentioned above, can help to restore normal serotonin production. These two supplements are just the tip of the iceberg.
Check Fit Recovery’s list of supplements that work best for supporting the brain-body system through recovery.
Conclusion
We hope you’ve taken useful information from this article. If you struggle with dependence on drinking, you will benefit from clicking around the articles on this website. If you struggle with drinking and you’re ready to transcend addiction forever, you have landed in the right place.
If you have any questions, please leave them in the comment box below.
___________________________________
Dr. Ken Starr is board-certified in both Addiction Medicine and Emergency Medicine, and diplomate of the American Board of Addiction Medicine. In addition to his work as the Addiction Medicine Director for Fit Recovery, he operates Ken Starr MD Wellness Group in Arroyo Grande, CA. His clinic offers advanced drug and alcohol detox methods, long-term recovery facilitation, and IV nutritional programs including NAD+ therapy.
Author
-
Dr. Ken Starr is board certified in both Addiction Medicine and Emergency Medicine, and diplomate of the American Board of Addiction Medicine. In addition to his work as the Addiction Medicine Director for Fit Recovery, he operates Ken Starr MD Wellness Group in Arroyo Grande, CA. His clinic offers advanced drug and alcohol detox methods, long term recovery facilitation, and IV nutritional programs including NAD+ therapy.
View all posts