
As with a refugee crisis or a hurricane, the collective knee-jerk reaction to America’s addiction epidemic is to demand billions of dollars of federal assistance. The issue transcends ideological boundaries: every political figure, from Nancy Pelosi to Donald Trump, seems to agree that the solution lies in achieving near-universal access to addiction treatment.
Yet what might the expected return on such a gargantuan investment look like? A typical one-month rehab stay costs $30,000, and outpatient treatment goes for at least $500 per day. The rehab industry has already grown from $20 billion in 2003 to over $35 billion in 2017. Over 90% of American rehab centers indoctrinate patients with the 12-step principles of AA, which itself has an estimated 5-10% success rate. Unsurprisingly, 80-90% of rehab patients relapse within a few months after discharge. These are the numbers that no one wants to talk about.
Meanwhile, alcohol continues to claim nearly 90,000 lives per year, with the alcohol addiction rate increasing from 9% in 2003 to nearly 13% in 2013. Drug overdoses reached an all-time high in 2015 and then increased another 19% in 2016 to reach 65,000 deaths, more than the number of American soldiers killed in the Vietnam War. No matter how much money we pour into addiction treatment, the industry in its current state cannot keep up with these frightening trends.
The good news is that substantial progress could be made simply by removing barriers to innovation in addiction recovery. Some of these barriers are legal, while others are stale assumptions that plague both government and the treatment industry, making the latter ripe for disruption.
The first obstacle to reducing relapse rates is the expansion of the War On Drugs itself. Instead of learning from its failure to make heroin (or any other drug) unavailable on the streets, our government has decided to pursue a ban of the only plant known to save heroin addicts from themselves.
This plant is called kratom, and over the past decade, hundreds of thousands of Americans have made tea from its leaves to eliminate opiate withdrawal and resume life as productive members of society. Thousands of former alcoholics have also warded off relapse with kratom for long enough to achieve a lifestyle that revolves around neither alcohol nor kratom.
One would expect a government that cares about the citizens it serves to encourage research into such a plant, perhaps crafting guidelines for consumer safety. Instead, the FDA has vilified kratom, recommending that the DEA designate it as a Schedule I substance as quickly as possible. Despite widespread protests that beat back a kratom ban in 2016, it appears that kratom may not remain legal for long.
If the DEA bans kratom, millions of nonviolent felons will be created overnight, including legions of Iraq War veterans – and elderly grandmothers. Up to a million ex-opioid addicts who use kratom for pain management will be faced with stark options: Suffer from excruciating pain, return to black market pills or heroin (or black market kratom), or purchase Suboxone, a powerful opioid maintenance drug approved by the FDA. I have no doubt that pharmaceutical lobbyists have their sights set on gaining a million new paying customers for their employers.
Kratom is not the only innovation from Nature herself that threatens Big Pharma and Big Government. New research shows that non-psychoactive CBD oil, which can be extracted from either marijuana or industrial hemp, has the potential to reduce neuro-inflammation, decreasing rates of drug and alcohol relapse as well as impulsive behavior. If the results of this animal research can be replicated in humans, we may soon discover that a 1-week administration of CBD oil gives people struggling with addiction a new lease on life for up to 5 months.
While 16 states have passed pro-CBD legislation and a 2014 Farm Bill was widely interpreted to legalize CBD extracted from hemp, the DEA recently stated that it does not regard any CBD oil as legal.
We should think about the deeper implications of kratom and CBD for addiction treatment. Switching to kratom from deadly pills, heroin, or alcohol is a form of harm reduction, which itself is a form of blasphemy in 12-step rehabs that preach total abstinence. When I attended inpatient rehab years ago for alcohol addiction, we were encouraged to laugh at people who used a program called Marijuana Maintenance to stay away from harder drugs or alcohol. “Marijuana might not kill you, but if you use it, you’re not really sober,” the counselor warned. A variation of the gateway drug theory was then used to preempt any further discussion of the potential benefits of marijuana or CBD.
I did not use marijuana to beat alcohol addiction, but who am I to pass judgment on others? And further – could the presence of CBD be the reason that marijuana is not known to be particularly addictive in the first place? In the absence of inflexible dogma, these questions would not be considered taboo among addiction counselors. And in the absence of the War On Drugs, the aforementioned research on CBD could have been performed in the U.S. many years ago.
Without arguing that no one is helped by AA, I think that it’s time to challenge that program’s monopoly on addiction treatment. Studies should be done on the psychological effects of diagnosing people with a permanent condition, telling them that they are “powerless” over it, and encouraging them to see the totality of their being through the bleak lens of their “disease.” In my experience, beliefs can easily become self-fulfilling prophecies.
Without arguing that no one needs inpatient treatment – severe alcohol withdrawal, for example, can be fatal – I believe that it’s time to challenge the idea that everyone with an addiction needs to spend weeks in expensive centers that often do little more than introduce people to a spiritual program that was intended to be free. Some people probably do benefit from spending time away from home, but busing them to outside meetings may not be the best use of money and time.
Government crowds out innovation in addiction treatment by perpetuating the status quo. Many local courts mandate rehab attendance or a set number of AA meetings, inflating the presumed efficacy of such “treatment” and oddly transforming judges into doctors who prescribe divine intervention. (One woman was ordered back to jail after her rehab center reported that she had failed to find a Higher Power in accordance with AA.) This practice violates AA’s own principles as a freely chosen organization, and it has been ruled unconstitutional several times.
For its part, the federal government fueled the rehab industry boom with a series of laws, including the “Parity Act” (MHPAEA) of 2008 and the Affordable Care Act of 2010, which created new streams of insurance money for a largely ineffective system. In “Covered California,” which covers virtually any treatment deemed to be addiction-related, we see an explosion of insurance fraud schemes, patient brokering, medical malpractice, and even human trafficking.
But there are reasons to be hopeful. A growing number of doctors are becoming better versed in medication-assisted treatment (MAT), which utilizes specific prescription drugs to help people break their addictions once and for all. The use of naltrexone for alcohol addiction, known as The Sinclair Method, has proven to be effective for many. The growth of MAT is one small step in the direction of viewing addiction as a biochemical disorder that can be managed and perhaps even resolved, rather than a disempowering “spiritual disease” that can never be overcome.
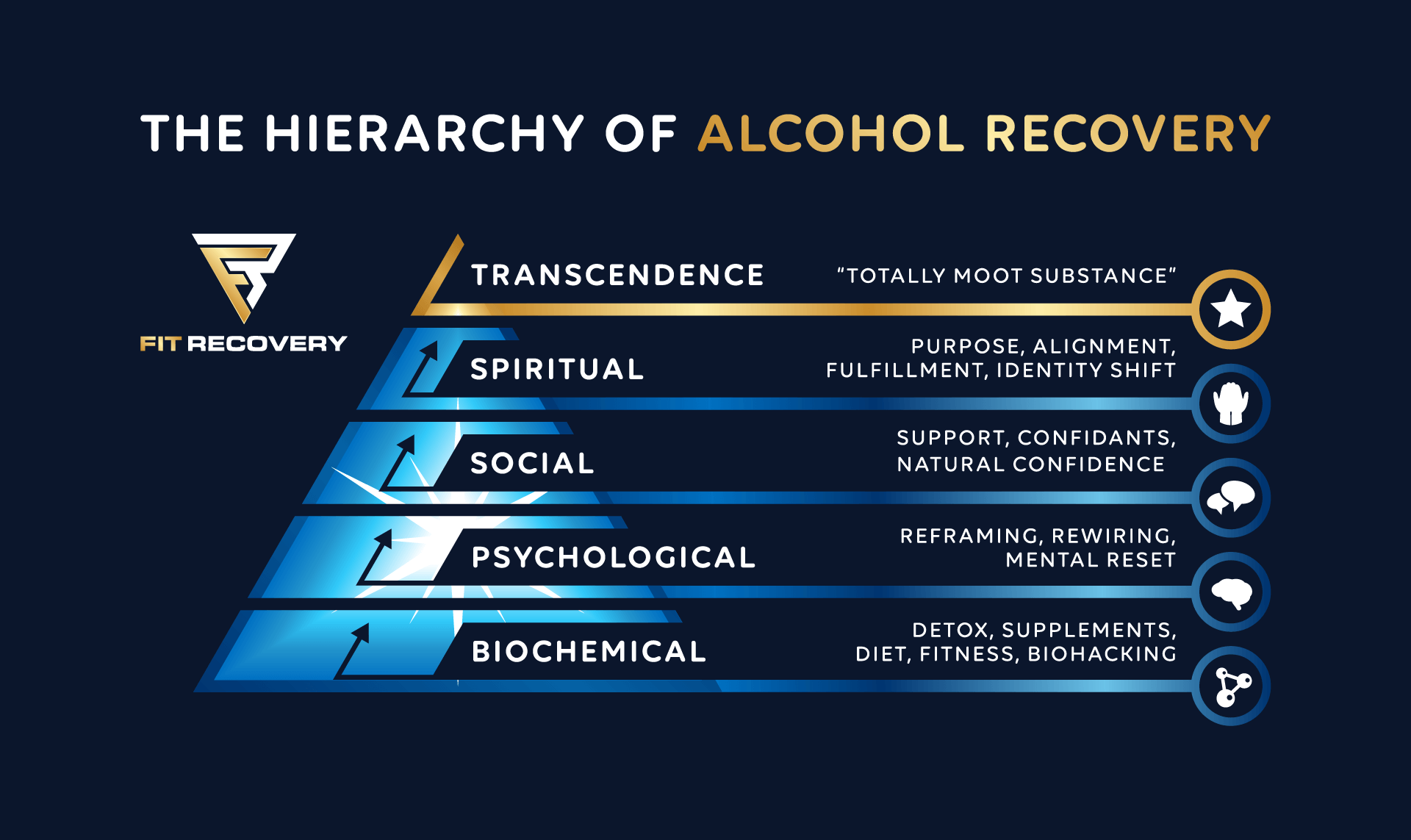
Moreover, just as the Internet saved kratom from an imminent ban in 2016 by enabling its widespread beneficiaries to organize rallies, so it has increased the ability of individuals in diverse places to share practical solutions for addiction. Lesser-known resources like SMART Recovery, Reddit forums, and opiate addiction support websites are beginning to get the attention they deserve. New apps are being invented that help people deal with the psychological aspects of beating addiction. This website, Fit Recovery, has helped tens of thousands of readers address physical gaps in their recovery, emphasizing the importance of nutrition and exercise for optimizing brain health and regaining long-term vitality.
I predict that sooner or later, the old paradigm will die, paving the way for cutting-edge science and practical approaches. AA will continue to have its place for people who need it, but alternatives will no longer be dismissed by treatment center authorities as routes to “jail, institutionalization, or death.” Whether the government ultimately respects our personal freedom to heal our bodies and brains with plants, if we so desire, remains to be seen.
Author
-
Chris Scott founded Fit Recovery in 2014 to help people from around the world dominate alcohol dependence and rebuild their lives from scratch. A former investment banker, he recovered from alcohol dependence using cutting-edge methods that integrate nutrition, physiology, and behavioral change. Today, Chris is an Alcohol Recovery Coach and the creator of an online course called Total Alcohol Recovery 2.0.
View all posts








Sorry Scott. There’s a reason AA and NA succeed so often–in the cumulative sense. You can go back multiple times without spending more than a token amount. You just can’t afford to do that at most residential treatment centers. AA/NA address the social nature of addiction. Addicts need social support to replace the camaraderie of addictive life, and AA/NA provides that for free–short, medium, and long term. As far as higher power, I do have problems with that concept, but the universe or greater consciousness can be a power greater than yourself. NA does a much better job including the… Read more »
Welcome e! I don’t have a problem with AA, social support, or even a higher power concept. Many people whose lives have been altered by this website attend AA, which helps them socially/spiritually but offers little guidance for feeling better physically. Perhaps that’s because AA was founded in 1935. Back then, no one knew about the associations between exercise and neurogenesis, gut health and brain function, supplementation and neurotransmitter levels, diet and energy levels. You don’t think anything has been discovered since 1935 that might be relevant for people struggling with addiction? Drugs with proven efficacy like naltrexone, gabapentin, baclofen,… Read more »